This is an online E log book to discuss our patient's de-identified health data shared after taking his/ her /guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
Here is a case I've seen:
A 67 year old man was brought to the hospital by his son with chief complaints of sudden onset weakness of left upper & lower limbs since last night associated with slurring of speech and deviation of mouth towards right.
History of present illness:
The patient was apparently asymptomatic 1day back,then developed sudden onset giddiness a/w fall and weaknes of left upper and lower limbs and deviation of mouth to right ,followed by slurring of speech since last night ,non progressive.pt. was taken to rmp,his BP was 150/100mmhg,he was then administered T.Amlong 30mg,pt. presented to our hospital after 12 hrs of onset of symptoms.
H/o difficulty in holding objects, difficulty in standing and walking
No H/o headinjury,LOC,nausea,
Vomitings,blurring of vision, involuntary micturition/defecation.
no h/o headache,
no difficulty in swallowing,
no h/o involuntary movements,fasiculations
No h/o loss of pain, temperature
No H/o palpitations,sweating,chest pain, breathlessness.
PAST HISTORY:
K/c/o HTN since 6 years and is on
T.Amlong OD, k/c/o COPD since 15 yrs,on budesonide& salbutamol nebulisation.
No h/o diabetes mellitus, epilepsy , chronic heart and kidney diseases, tuberculosis, thyroid disorders.
No similar complaints in the past.
H/o fall from a tree 3yrs back with no significant injuries.
No H/o previous surgeries and blood transfusion.
PERSONAL HISTORY:
Diet: mixed
Appetite: normal
Sleep: adequate
Bowel and bladder movements: regular.
No addictions,occasional toddy drinker.
Lives with wife and 2 sons.
FAMILY HISTORY:
No significant family history.
DRUG HISTORY:
allergic to T.Combiflam(exacerbates COPD)
GENERAL EXAMINATION:
Patient is drowsy
Moderately built and moderately nourished.
No signs of pallor, icterus, cyanosis , clubbing, koilonychia, generalised lymphadenopathy, bilateral pedal edema.
VITALS:
Temperature: afebrile
Pulse rate: 68 bpm,irregularly irregular
BP: 140/90 mm of hg
RR: 15 cycles per min.
Sp02 : 98% at room temperature
GRBS: 100 mg/dl
SYSTEMIC EXAMINATION:
CNS
Higher mental functions:
pt.is drowsy,oriented to time, place,person. slurred speech.
Remote & recent memory - intact
Pupils - NSRL
Spinomotor :
no wasting/ thinning of muscles. No pain, fatigue and fasciculations.
Right Left
Bulk :
Upper limb Normal Normal . Lower limb . Normal. Normal
Tone:
Upper limb:. Normal. Decreased .
Lower limb:. Normal. Decreased .
Power:
Upper limb:. 5/5. 0/5
Lower limb:. 5/5. 0/5
Hand grip : 100% . 0%
following commands
Motor system
Reflexes:
Superficial reflexes: normal
Deep tendon reflexes:
Biceps:. 2+. 2+
Triceps:. 2+ 2+
Supinator:. 2+ 2+
Knee:. 2+ 2+
Ankle:. -. -
Plantar:. Flexor extensor
Sensory system: right Left
Fine touch + +
Vibration + +
Position sense + +
Crude touch + +
pain and temperature + +
Rhomberg's - absent
Cerebellum:
Nystagmus -ve
Pendular knee jerk -ve
Rebound phenomenon -ve
Dysdiadochokinesia -ve
Finger nose incoordination-ve
Finger finger incoordination-ve
Gait - couldn't be elicited
Cranial nerve examination:
I : intact
II : visual acuity 6/6
Colour vision normal
III,IV,VI : normal pupil size
No nystagmus,ptosis,eyemovements normal
V: Sensory - normal
Motor - normal
Corneal & conjunctival reflexes - normal
Vll: Deviation of angle of mouth towards right, Able to close eyes.
frowning present on both sides of forehead
VIII : normal.
IX,X: Uvula- not visualised,gag reflex +
XI: normal
XII: tongue- tone normal,no deviation
ANS:regular bladder movements. No sweating and palpitations.
Meninges: no signs of meningeal irritation(fever, headache, neck stiffness, nausea and vomitings)
PERABDOMINAL EXAMINATION:
Shape of abdomen: scaphoid
No tenderness and local rise of temperature.
No palpable masses.
Hernial orifices normal.
No free fluid and bruit.
Liver and spleen : not palpable.
Bowel sounds: normally heard.
RESPIRATORY SYSTEM:
Position of trachea: central
No wheeze and dyspnea.
Bilateral air entry present.
Normal vesicular breath sounds heard.
No adventitious sounds.
CVS:
S1 and S2 heard.
No murmurs.
Based on the clinical findings,the following investigations were sent:
CBP
CUE
RFT
RBS
FLP
ECG
2D ECHO
Troponin I - negative
FUNDOSCOPY- B/L IMSC
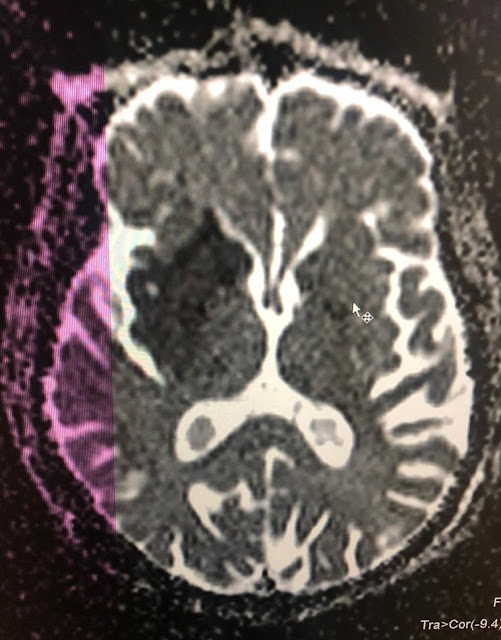
MRI BRAIN plain
USG abdomen
CAROTID DOPPLER
Day 1
DIAGNOSIS:
Ischemic CVA with left sided Hemiplegia with UMN facial palsy 2° to infarct In ? MCA territory
K/C/O HTN & COPD
Treatment:
1. Ryle's tube feed - 200ml milk 2nd hourly with proteinex powder
100 ml water hourly
|
Day3 - soft diet --- regular diet
2. INJ MANNITOL 20mg/IV/TID
3. INJ PANTOP 40mg IV OD
4. T. ECOSPIRIN 300mg OD/RT/STAT
|
150 mg OD
5. T. CLOPIDOGREL 150mg OD/RT/STAT
|
75 mg OD/RT
6. T.ATORVAS 20mg H/S/RT
7. Physiotherapy for left UL & LL
8. Frequent mobilization
9. Vitals monitoring hrly,I/O charting












Comments
Post a Comment